Responses essay paper
Responses
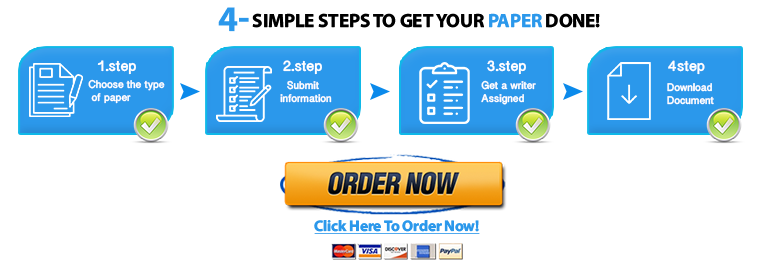
ORDER A PLAGIARISM FREE PAPER NOW
Response1
The National Council of State Boards of Nursing (NCSBN) clinical judgment measurement model is a tool used to assist nurses in critically thinking and forming solutions. Efficient nurses use this line of thinking while analyzing data, prioritizing hypotheses, generating solutions, and evaluating Responsesoutcomes. Thinking back to a time when I used the steps in this model, I was actually a certified nursing assistant working with a client in assisted living. In this scenario, a coworker and I had walked in on a client with type two diabetes mellitus who was diaphoretic, shaky, confused, pale, and tachycardic. Knowing that these symptoms were concerning especially with a diagnosis of diabetes, I knew we had to intervene fast and efficiently.
Step one in the clinical judgment model begins with recognizing cues. The importance of the cue collection stage in clinical judgment and reasoning cannot be underestimated. If early subtle cues are missed, this can lead to adverse patient outcomes (Levett-Jones, 2018). The patient cues I observed in this scenario were the client’s diaphoresis, shaking, confusion, pallor, and fast heart rate. To place these observations in order of priority, I used the ABC pneumonic: (A): airway, (B): breathing, and (C): Circulation (Ignatavicius, et al., 2021). When using this method to prioritize cues, I would place them in the order of 1. Tachycardia, 2. Pallor, 3. Diaphoresis, 4. Shaking, and 5. Confusion. Responses
Step 2 in the clinical judgment model is to create and prioritize hypotheses. Based on the analysis of the given cues, I formulated three hypotheses. Since he was a type 2 diabetic, the first hypothesis I generated was that this client experiencing tachycardia, pallor, diaphoresis, shaking, and confusion was hypoglycemic. The second hypothesis I generated was that the client experiencing tachycardia, pallor, diaphoresis, shaking, and confusion was experiencing anxiety. The third hypothesis I generated was that this client experiencing tachycardia, pallor, diaphoresis, shaking, and confusion was developing dementia as he was 80 years old and has a family history of dementia and Parkinson’s disease. Responses
The third step in the clinical judgment model is prioritizing hypotheses. The two priority hypotheses I chose for this patient were hypoglycemia and anxiety. The reason I prioritized the first hypothesis is that the Identification of a hypoglycemic patient is critical due to potential adverse effects including coma and/or death (Matthew, et al., 2022). The reason I chose anxiety over dementia was that anxiety causes high cortisol levels. In moderation, cortisol can be healthy as it triggers the ‘fight or flight’ response from our central nervous system. However, when the body is exposed to high cortisol levels for extended periods of time like in cases such as anxiety, this can lead to fatigue, high blood pressure, headaches, depression, poor sleep, etc. (Premier Health, 2017).
Step 4 of the clinical judgment model is to generate solutions. In this stage, it is important to understand the priority update that needs to be made to the plan of care and priority interventions. The priority intervention for this patient was to notify the registered nurse on call, administer fruit juice or other readily absorbable carbohydrate sources, and call emergency medical services or 911. Severe hypoglycemia can be treated with intravenous (IV) dextrose followed by an infusion of glucose. ResponsesFor conscious patients able to take oral medications, readily absorbable carbohydrate sources (such as fruit juice) should be given (Matthew, et al., 2022). Regular blood sugar checks should be implemented for this patient’s plan of care as well as regular wellness checks. Prior to this instance, they were not regularly checked on. Afterward, they had hourly checks by staff.
The last stage of the clinical judgment model is to evaluate outcomes. What went well in this situation is how quickly my coworker and I responded to the scenario. We recognized the client’s symptoms and put them together with the fact that he was diabetic. Knowing that these symptoms aligned with hypoglycemia, we took his blood sugar which was approximately 62 mg/dL. We administered cranberry juice that was in his fridge and called 911. Using the clinical judgment model, we came to the correct conclusion and potentially saved this client’s life. Understanding the steps to this model is crucial when it comes to critical thinking and providing the best outcomes for patients.
Response2
I will never forget this day. I can remember every detail of this day. It was during the noon hour, there was an overhead page. “Medical Emergency in the parking lot.” Everything after happened so fast, even though it was over a 2.5-hour period. I grabbed a wheelchair on my way out and a father and his son were in front of the door. The father stated, “he has carbon monoxide poising” several times. The son was in the truck saying, “somebody helps me I am going to die” repeatedly, and violented started to vomit. This was happening simultaneously; I was unsure who to address as this was clearly a medical emergency. I had an assumption of drug use in the patient due to his actions. As I was wheeling him into the procedure room of the clinic, several staff members joined me, and I was attempting to give them all the information I had based on the conversation in the parking lot. At this point, everyone understood that it was possible carbon monoxide poising as he was working with machinery in an enclosed space and became nauseous and became confused. Responses
Once we were in the procedure room the patient coded. We immediately began medical emergency interventions our clinic has EKG, and CPR/AED making limited what we could do for the patient. It was chaotic a cop was in and out of the room, and other staff were in and out of the room I asked several times if we should administer Narcan and was told no every time. We brought him back 3 times and he immediately coded again. This continued for about 45 minutes until the ambulance arrived. In the meantime, a helicopter was on its way to meet the ambulance and when the ambulance arrived, they were short-staffed. I climbed into the ambulance with one of the cops and one EMT member and continued to administer CPR. I somehow ended up on the ambulance once it started moving as they were short. Once parked some distance from the clinic I stayed in the ambulance and assisted with CPR while as many of his loved ones as possible, came into and stood outside of the ambulance. They kept asking the patient “why would you do this?” and sobbing and then his father said, “just stop he is not coming back, please.” I didn’t listen or respond, I just kept performing CPR. Finally, the helicopter medicine team came and called it-and we stopped CPR. I apologized to the family and left the ambulance and walked back to the clinic. On my way back I began to cry and told myself to stop. By the time I entered the clinic I composed myself and went to our huddle room out of patient and staff sight. Immediately, my nurse manager asked me if I was in the ambulance the whole time. I said “yes, they were short” to which she responded, I just want to let you know that is against policy to leave the clinic with a patient in the ambulance. What?! This was the worst experience I have ever had, and I was simply trying to save him, and I couldn’t despite desperately attempting due to extenuating circumstances. I broke out in tears and stated I would do it again even though I couldn’t save him.
After the situation, we had a debriefing to see what could have been done differently. We concluded that communication was essential in this situation because there were 2 people in the facility doing CPR for the whole period prior to the ambulance arriving (I was one of them). Then I ended up in the ambulance with some staff not knowing, due to lack of communication.
Once I returned home, I lost it. I kept running the situation over and over in my head wondering what could have been done differently to have had a different outcome. I symptom researched symptoms and treatments. I talked to two close co-workers who were involved in the situation. I couldn’t stop the thoughts or frustration of failing this patient. I understood that if I could have asked the patient questions and focused on him, I could have possibly gotten pertinent information to help him.
I feel now that while there were many instances of ineffective communication, knowing that I can use my voice to bring comfort to others in emergency situations by controlling my actions and emotions the situation in a professional manner and following through. I also learned it was not my fault CPR was not effective however, I feel I should have advocated for the patient to receive the Narcan upon presenting to the clinic. The family refused an autopsy so, we will never know the actual cause of his death. However, I did everything I could to save the patient. I learned that understanding cues, and communication is important in every situation and is essential for optimal outcomes for everyone involved.
The external clues in this scenario include the patient’s presenting symptoms, the communication from those who brought him, and the awareness that this was an emergent situation as evidenced by the preceding factors.
The internal cues in this scenario include the indication of the need for CPR/AED, and EKG Narcan from myself in order to best treat the patient. In addition, my response was to stay with the patient to continue CPR when needed when the ambulance staff was short to ensure that interventions for the patient continued.
The following hypotheses were utilized in this scenario:
The patient’s presenting symptoms are indicative of drug overdose as evidenced by confusion, vomiting, and eventual loss of consciousness. Understanding the reason for the symptoms in the patient will better equip medical staff in ADPIE.
The patient’s symptoms of loss of consciousness, pulselessness, and termination of breathing indicate medical intervention to resuscitate as evidenced by these symptoms. Understanding the priority to stabilize the patient to maintain ABCs to prevent further injury and revive the patient. Responses
Ineffective communication regarding the reason for presenting symptoms, the role of medical staff, and may have changed the outcome for the patient as evidenced by the patient succumbing to his symptoms. Proper communication will result in an optimal outcome for the patient as all aspects of care are covered through proper communication with those involved in the situation. Responses
Action and Evaluation
The ability for any medical staff to deliver Narcan to patients presenting with drug overdose symptoms should be implemented in order to reduce the risk of death to those who do not give information stating they have been using narcotics-especially in the occurrence of loss of consciousness. Evaluation should occur once the medication is administered. Basic life support measures in this scenario should continue throughout the process and remain in place if the patient is unresponsive to Narcan (dhs.org, 2022).
Understanding that CPR/AED measures should continue until the patient is revived or proper medical personnel calls for the death of the patient. Facility policy should reflect this as our duty to patient safety and advocacy should be prioritized in this scenario. Once the policy is adjusted and implemented patient safety and advocacy will prevail in more situations. If the policy cannot change staff should utilize nursing judgment and not be penalized in extreme situations for non-adherence to the policy (AHA, 2000).
Response3
Pharmacological – Some pharmacological treatment include administering epidural analgesia or administering nitrous oxide gas for pain relief. Epidurals are considered the most effective and recommended method of pain relief (Czech et al, 2018). Th\is method of pain relief had the lowest rate of pain during each stages of labour (Czech et al, 2018). There were some studies that showed an epidural has a greater risk for performing instrumental vaginal delivery (Czech et al, 2018). Some side effects include back pain, headaches, (Czech et al, 2018). There is always a chance at developing a fever due to the epidural and while being pregnant and having a fever that can increase the baby being born with poor muscle tone, breathing issues, and lower Apgar scores (Birth injury, 2022). Another method of pain delivery includes nitrous oxide gas. This method has relieved pain with no adverse foetal outcomes (Czech et al, 2018). This is also the second most common used pain relief behind the epidural, but most women have been satisfied with their experience with it (Czech et al, 2018). There was records that stated this was the worst reduction of pain during the second and third stages of labour, compared to the epidural (Czech et al, 2018). When combined with TENS or water immersion the results were better (Czech et al, 2018).
Non-pharmacological – Some non-pharmacological pain relief includes TENS and water birth or immersion. Water birth has been around for a long time, but just recently has been becoming more popular (Czech et al, 2018). During this process, the hydrostatic pressure is lower than the intraabdominal pressure, which eases the breathing and changing of positions (Czech et al, 2018). During contractions, the pelvic tissues are more elastic and flexible, which reduces the amount of pain (Czech et al, 2018). Another form of pain relief is transcutaneous electrical nerve stimulation or other words TENS. This is considered the most least satisfying methods, but when combined with gas control, the effects increased (Czech et al, 2018). during the first stages of labour, TENS was successful, but later stages it was minimizing or postponing the pharmacological analgesia (Czech et al, 2018).
Response4
Pharmacological interventions include narcotics, which are preferably given early in the laboring process as they have been known to slow labor if given prior to the woman being 3cm dilated and include butorphanol, morphine, nalbuphine, meperidine and fentanyl. As these decrease pain sensation in the mother and cause the system to relax, the same happens with the fetus with usual signs of respiratory depression.
Another example of pharmacologic pain relief is by using an anesthetic. This can range from topical lidocaine to general anesthesia. With general anesthesia, a natural, vaginal birth is not accomplished as the muscles do not contract to push the fetus into and through the birth canal which then requires a forceps or vacuum delivery or possibly a c-section. For the fetus, CNS depression is often seen with delayed reactions for the first few days of life. What I did not know is there are a few local anesthetics (blocks) that are used such as lidocaine injected into the superficial nerves along the vulva and a pudendal block where an injection is placed into the vagina. Both sound awful as I remember the burning and pain of the local anesthetic I received when needing to be stitched after my tear.
Non-pharmacologic interventions are numerous and not everyone responds to the same method(s). One of the more effective non-pharmacologic interventions is that of touch and massage as this helps to irritate the nerve fibers and block pain signals from reaching the brain. Additionally, having the pressure that massage provides is often very relaxing to a woman and its at this point that deeper and harder mean exactly that! Additionally, music, breathing exercises, aromatherapy, use of a birthing ball, and water are great additives in pain relief and distraction.
Reply Post –
• Discuss three potential barriers that you would anticipate when providing care to Jose based on his age and culture.
• Provide an example of how you would overcome each of the three barriers through the implementation of multidimensional care strategies. Responses
Response5
We are presented with a 55-year-old male patient with scrotal edema, urine retention, and hematuria. The pathological processes that he may be experiencing could be related to the patient possibly suffering from benign prostatic hypertrophy(BPH), which can clog the urethra and cause varicose veins of the local veins, resulting in hematuria and difficulties urinating, as well as being linked to infectious processes that might cause testicular edema (Workman, 2021).
It is a common condition among males as they become older, mainly beyond the age of 40. Because of the enlargement of the prostate gland, the patient has urinary symptoms such as urine retention. This expansion gradually compresses the urethra, eventually producing partial or full obstruction of urine flow out of the bladder. Hematuria is frequent with untreated BPH related to hypervascularity of the prostate, which causes blood vessels to be readily ruptured, and because the prostate is directly involved in the urinary system, any blood leakage caused by this enlargement would be evacuated through the urethra (Workman, 2021).
To effectively deliver multidimensional care, it is necessary to first establish trust and rapport with the patient. Assist in creating an environment in which the patient feels safe and comfortable. Because the patient speaks minimal English, it is necessary to bring in a translator to overcome this language barrier in order to successfully offer quality care and address his overall needs. Also, getting the patient in touch with some resources due to limited finances could be an option as he speaks limited English he may have trouble on his own finding these resources.
Response6
Disease Process + Signs and Symptoms – After reading the case study, I feel Jose’s complaints of edema of the scrotum, urinary retention, and hematuria are related to benign prostatic hyperplasia (BPH). Jose is 55 years old. Men who are over the age of 50 are at an increased risk for BPH. (Urology Care, 2021) BPH can lead to bladder damage and infection, which can cause blood in the urine. (Urology Care, 2021) Due to the delay in seeking care, I feel an infection has developed, thus explaining blood in Jose’s urine. I also suspect Jose may also have prostate cancer. BPH isn’t cancer, however, prostate cancer can happen at the same time. (Urology Care, 2021) Prostate cancer and BPH have similar symptoms.
• BPH: hesitancy, weak stream, urinary retention, straining to begin urination, postvoid residual, and hematuria when the infection is present. (Urology Care, 2021)
• Prostate Cancer: hematuria (late sign), painful or burning urination, weak stream, hesitancy, and frequency. (John Hopkins Medicine, 2021)
Men who are older than 65 are at an increased risk for prostate cancer, with the average age of diagnosis being 66. (Ignatavicius, 2022) Besides age, having a family history of prostate cancer could put Jose at a greater risk as well. But with what has been presented in the case study, we don’t know exactly Jose’s family history.
Multidementional Care – The first thing I would do is get an interpreter involved since Jose speaks limited english. I would want Jose to understand my education about the disease process (after he was diagnosed of course), and what resources and treatments are available to him. As Jose’s nurse I would not only be an advocate for him, but I would also help him navigate any referrals, tests, and treatments he may have. A social worker is somebody I would also like to get involved to help Jose and his family when it comes to their finacial situation and being able to afford the care Jose may need. If Jose were to be diagnosed with prostate cancer (hopefully not), I would include a psychologist and/or a psychiatrist to help him (and his family) cope with his new diagnosis.